Concussion Symptoms and Recovery: Complete Guide for Parents and Coaches
Understanding concussion symptoms is critical for every parent and coach involved in youth sports. Concussions are one of the most common yet misunderstood injuries in youth sports. Every year, thousands of young athletes across Canada experience concussions, yet many parents, coaches, and athletes lack critical knowledge about what concussions are, how they happen, and how to manage them safely. According to Parachute Canada, concussions account for approximately 20% of all sport-related injuries among youth athletes. In Ontario, Rowan’s Law mandates that all sport organizations implement concussion protocols, making concussion education and management a legal requirement. Understanding concussion symptoms, concussion recovery, and prevention strategies is essential for protecting athletes and ensuring safe participation in sports.
What Is a Concussion?
A concussion is a type of traumatic brain injury caused by a blow to the head, face, neck, or body that transmits force to the brain. This impact causes the brain to move rapidly inside the skull, leading to chemical changes in the brain and sometimes stretching or damaging brain cells.
Key characteristics of concussions:
- Concussions are functional injuries, not structural—they affect how the brain works rather than causing visible damage on standard imaging tests
- They can occur with or without loss of consciousness (in fact, most concussions do not involve losing consciousness)
- Symptoms may appear immediately or develop over hours or days following the injury
- Each concussion is unique, with varying concussion symptoms and recovery timelines
- Concussions are considered mild traumatic brain injuries, but “mild” doesn’t mean insignificant
The brain injury occurs when the brain’s normal function is disrupted, affecting everything from balance and coordination to memory, concentration, and emotional regulation. Understanding what is a concussion helps parents and coaches recognize when medical evaluation is needed.
How Do Concussions Happen? Common Causes in Youth Sports
Concussions in sports can result from various mechanisms, and understanding how they occur helps with concussion prevention and early recognition of signs of a concussion.
Common Causes of Sport-Related Concussions:
Direct Impact to the Head:
- Collisions with other players (most common in contact sports like hockey, football, rugby)
- Being struck by equipment (pucks, balls, sticks)
- Falls resulting in head impact with the ground or playing surface
- Contact with goal posts, boards, or other fixed structures
Indirect Force Transmission:
- Body checks or tackles that cause whiplash-like motion
- Sudden acceleration or deceleration of the head
- Rotational forces that twist the brain inside the skull
High-Risk Sports and Activities: Research shows that hockey, football, and soccer account for over 60% of sport-related concussions in Canadian youth. Other high-risk activities include:
- Contact sports: Hockey, football, rugby, lacrosse, boxing
- Collision sports: Soccer (especially heading), basketball
- Individual sports: Skiing, snowboarding, skateboarding, cycling
- Recreational activities: Playground activities, cheerleading, gymnastics
It’s important to note that concussions in sports don’t only happen in contact activities. Any sport or activity where there’s risk of falling, collision, or impact can result in a concussion.
Recognizing Concussion Symptoms
Concussion symptoms vary widely between individuals and can affect physical, cognitive, emotional, and sleep-related functions. Early recognition of signs of a concussion is critical for proper concussion management and recovery.
Physical Symptoms:
- Headache or pressure in the head
- Dizziness or balance problems
- Nausea or vomiting
- Blurred or double vision
- Sensitivity to light or noise
- Feeling sluggish, foggy, or groggy
- Fatigue or low energy
Cognitive Symptoms:
- Difficulty concentrating or remembering
- Confusion or feeling “in a fog”
- Slowed thinking or processing
- Difficulty with problem-solving
- Feeling mentally “off”
Emotional Symptoms:
- Irritability or mood changes
- Increased emotional responses
- Nervousness or anxiety
- Sadness or depression
Sleep Disturbances:
- Sleeping more than usual
- Sleeping less than usual
- Difficulty falling asleep
- Drowsiness
Red Flag Symptoms Requiring Immediate Emergency Care:
- Neck pain or tenderness
- Severe or increasing headache
- Seizures or convulsions
- Loss of consciousness
- Repeated vomiting
- Increasing confusion or irritability
- Weakness or numbness in arms or legs
- Slurred speech
- One pupil larger than the other
If any red flag symptoms appear, call 911 or go to the nearest emergency department immediately. These signs of a concussion indicate serious injury requiring emergency medical attention.
Concussion Symptoms in Children vs. Adults: What Parents Should Know
Concussion symptoms in children and adolescents often differ from adults, and young athletes require more conservative concussion management due to their developing brains.
Unique pediatric concussion symptoms:
- Increased irritability or crankiness
- Changes in eating or sleeping patterns
- Loss of interest in favorite activities
- Difficulty with schoolwork or concentration
- Appearing dazed or confused more easily
- Excessive crying or inability to be consoled
Why children take longer to recover: Children’s brains are still developing, making them more vulnerable to concussion effects and requiring longer concussion recovery periods. Research shows that pediatric concussion recovery averages 3-4 weeks compared to 2-3 weeks in adults.
Special considerations for young athletes:
- More conservative return-to-play after concussion timelines
- Modified school accommodations during concussion recovery
- Close monitoring for emotional and behavioral changes
- Lower threshold for medical evaluation and concussion assessment
Parents should never assume their child will “tough it out” or recover as quickly as an adult athlete. Pediatric concussions require specialized concussion assessment and management by healthcare professionals experienced in youth concussion treatment.
Concussion Risks: Short-Term and Long-Term Effects
Understanding concussion risks helps emphasize why proper concussion management and prevention are non-negotiable for athlete safety.
Short-Term Risks:
Second Impact Syndrome: The most serious short-term risk occurs when an athlete sustains a second concussion before fully recovering from the first. Second Impact Syndrome can cause rapid and severe brain swelling, potentially leading to catastrophic injury or death. This rare but devastating condition underscores why athletes must be fully cleared before return to play after concussion.
Prolonged Symptoms: Returning to activity too soon can prolong concussion symptoms and delay concussion recovery. Athletes who don’t rest adequately often experience symptoms for weeks or months longer than necessary, sometimes developing post-concussion syndrome.
Increased Vulnerability: A brain that hasn’t fully healed is more susceptible to additional concussions, even from lesser impacts. Studies indicate that athletes with a history of concussion are 3-6 times more likely to sustain another concussion.
Long-Term Risks:
Cumulative Effects: Multiple concussions over time can lead to cumulative brain damage. Research shows that athletes with a history of concussions are at higher risk for:
- Longer concussion recovery times from subsequent injuries
- Persistent post-concussive symptoms
- Cognitive difficulties later in life
- Mental health challenges
Chronic Traumatic Encephalopathy (CTE): While still being researched, repeated head impacts and concussions may contribute to CTE, a degenerative brain condition associated with memory loss, confusion, depression, and dementia.
Academic and Social Impact: Concussions affect school performance, social relationships, and quality of life during the critical developmental years of childhood and adolescence.
Typical Concussion Recovery Timeline
Most concussions follow a predictable concussion recovery pattern, though individual experiences vary significantly. Research published in the British Journal of Sports Medicine shows that 80-90% of concussions resolve within 2-4 weeks with proper concussion management and treatment.
Recovery Phases:
Immediate Phase (0-48 hours):
- Complete physical and cognitive rest
- Concussion symptoms typically most severe
- No screens, reading, or stimulating activities
- Close monitoring for worsening symptoms
Early Recovery (2-7 days):
- Gradual return to light daily activities as tolerated
- Concussion symptoms should begin improving
- No sports or high-risk activities
- Modified school attendance if needed
Progressive Recovery (1-4 weeks):
- Most athletes complete concussion recovery within 2-4 weeks
- Gradual increase in cognitive demands
- Step-wise return to physical activity (only after symptom-free)
- Medical clearance required before return to sport
Extended Recovery (Beyond 4 weeks):
- 10-20% of concussions result in persistent symptoms (post-concussion syndrome)
- Requires specialized medical concussion assessment and treatment
- May need comprehensive rehabilitation program
Frequently Asked Questions About Concussions
What are the most common concussion symptoms?
The most common concussion symptoms include headache or pressure in the head, dizziness, confusion, nausea, sensitivity to light or noise, and difficulty concentrating. Physical, cognitive, emotional, and sleep-related symptoms can all indicate a concussion. Concussion symptoms may appear immediately or develop over hours or days after the injury.
How long does it take to recover from a concussion?
Most athletes complete concussion recovery within 2-4 weeks. The immediate phase (0-48 hours) requires complete rest, followed by early recovery (2-7 days) and progressive recovery (1-4 weeks). However, 10-20% of concussions result in persistent symptoms beyond 4 weeks (post-concussion syndrome), requiring specialized medical concussion treatment. Children and adolescents often take longer for concussion recovery than adults.
What should you do immediately after a concussion?
Immediately remove the athlete from play and do not allow return to play after concussion the same day. Monitor for red flag concussion symptoms requiring emergency care (severe headache, repeated vomiting, seizures, loss of consciousness). Seek concussion assessment by a healthcare professional trained in concussion management. Ensure complete physical and cognitive rest for the first 24-48 hours as part of initial concussion treatment.
Can you sleep with a concussion?
Yes, sleep is crucial for brain healing after a concussion. The outdated advice to wake someone every hour is no longer recommended unless specifically instructed by a doctor. Rest and sleep help the brain during concussion recovery. However, monitor the person for worsening concussion symptoms and seek emergency care if red flag symptoms develop.
What is Second Impact Syndrome?
Second Impact Syndrome occurs when an athlete sustains a second concussion before fully recovering from the first. This rare but devastating condition can cause rapid and severe brain swelling, potentially leading to catastrophic injury or death. This is why athletes must be fully cleared by a healthcare professional before return to play after concussion.
Do helmets prevent concussions?
No, helmets cannot prevent concussions in sports, though they do reduce skull fractures and severe brain injuries. The brain still moves inside the skull during impact regardless of helmet use. Helmets are important safety equipment for concussion prevention of severe injuries, but they don’t eliminate concussion risk.
When can an athlete return to play after a concussion?
Athletes can return to play after concussion only after they are completely free of concussion symptoms at rest AND have completed a graduated 6-step return-to-play protocol supervised by healthcare professionals. This concussion recovery typically takes 2-4 weeks minimum. Athletes must obtain medical clearance from a physician or nurse practitioner before returning to competition.
What are the long-term effects of multiple concussions?
Multiple concussions can lead to cumulative brain damage, including longer concussion recovery times, persistent post-concussive symptoms, cognitive difficulties, mental health challenges, and potentially Chronic Traumatic Encephalopathy (CTE). This is why proper concussion management and preventing premature return to play after concussion are critical.
How do you know if a concussion is serious?
Red flag concussion symptoms indicate a serious injury requiring immediate emergency care: neck pain, severe or worsening headache, seizures, loss of consciousness, repeated vomiting, increasing confusion, weakness or numbness in limbs, slurred speech, or unequal pupil size. Call 911 if any of these signs of a concussion appear.
What is post-concussion syndrome?
Post-concussion syndrome occurs when concussion symptoms persist beyond 4 weeks. Approximately 10-20% of concussions result in persistent symptoms requiring specialized medical concussion assessment and comprehensive rehabilitation. Symptoms may include ongoing headaches, dizziness, cognitive difficulties, and emotional changes requiring extended concussion treatment.
Concussion Prevention and Management: Evidence-Based Solutions
While concussions cannot be completely eliminated from sports, evidence-based strategies can reduce risk and minimize impact when injuries occur through effective concussion prevention and management.
Prevention Strategies:
Education and Awareness:
- Teach athletes, coaches, and parents to recognize concussion symptoms and signs of a concussion
- Emphasize the importance of reporting concussion symptoms immediately
- Create a culture where athlete safety trumps competition
- Provide annual concussion education for all stakeholders
Proper Technique and Training:
- Teach safe playing techniques that reduce head impact risk for concussion prevention
- Emphasize proper tackling, checking, and heading techniques
- Strengthen neck muscles to reduce head acceleration during impact
- Implement age-appropriate contact rules
Rule Enforcement and Modification:
- Enforce rules against dangerous play (checking from behind, targeting the head)
- Consider rule modifications that reduce head impact exposure
- Implement age-appropriate contact limitations
- Penalize dangerous play consistently
Equipment Considerations:
- Ensure properly fitted, certified helmets for sports requiring them
- Replace damaged or expired equipment
- Understand that equipment reduces some risks but doesn’t prevent concussions
- Use mouthguards in appropriate sports
Minimizing Impact When Concussions Occur:
Immediate Recognition and Removal: The most critical factor in concussion management is immediate recognition of concussion symptoms and removal from play. Athletes suspected of having a concussion should never return to activity the same day.
Proper Medical Evaluation: All suspected concussions require concussion assessment by a healthcare professional trained in concussion management. This ensures accurate diagnosis and appropriate concussion treatment planning.
Comprehensive Documentation: Detailed documentation of the injury, concussion symptoms, and recovery progress protects athletes and organizations while ensuring continuity of care across healthcare providers, coaches, and parents.
Graduated Return-to-Play Protocol: Following evidence-based return-to-play after concussion protocols ensures athletes don’t return to sport until their brains have fully healed, reducing risk of re-injury and prolonged concussion symptoms.
Access to Healthcare Professionals: Athletes recovering from concussions benefit from guidance by healthcare professionals who can monitor concussion symptoms, provide concussion education, and make informed clearance decisions.
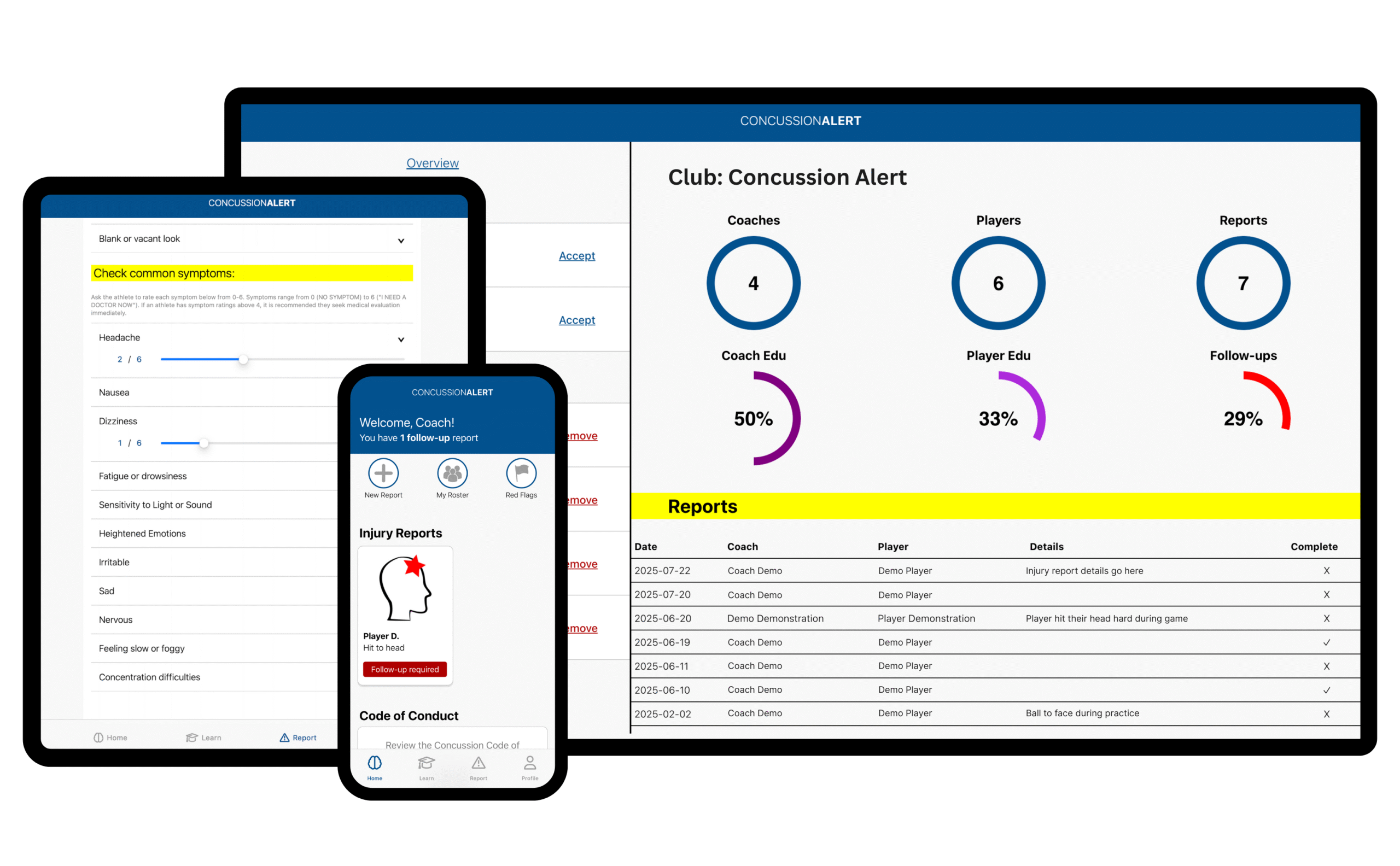
How CONCUSSIONALERT Improves Concussion Recovery and Safety
CONCUSSIONALERT provides sport organizations with a complete system for concussion prevention where possible and effective concussion management when they occur.
Education That Protects:
CONCUSSIONALERT ensures every coach, parent, and athlete receives annual concussion education based on current best-practice guidelines and Rowan’s Law requirements. The platform tracks completion automatically, ensuring 100% compliance and creating a culture of concussion awareness.
What’s included:
- Ontario concussion safety resources and Rowan’s Law compliance training
- Recognition of concussion symptoms and red flag signs of a concussion
- Proper response protocols when concussions are suspected
- Understanding of return-to-play after concussion requirements
- Annual refresher training with completion tracking
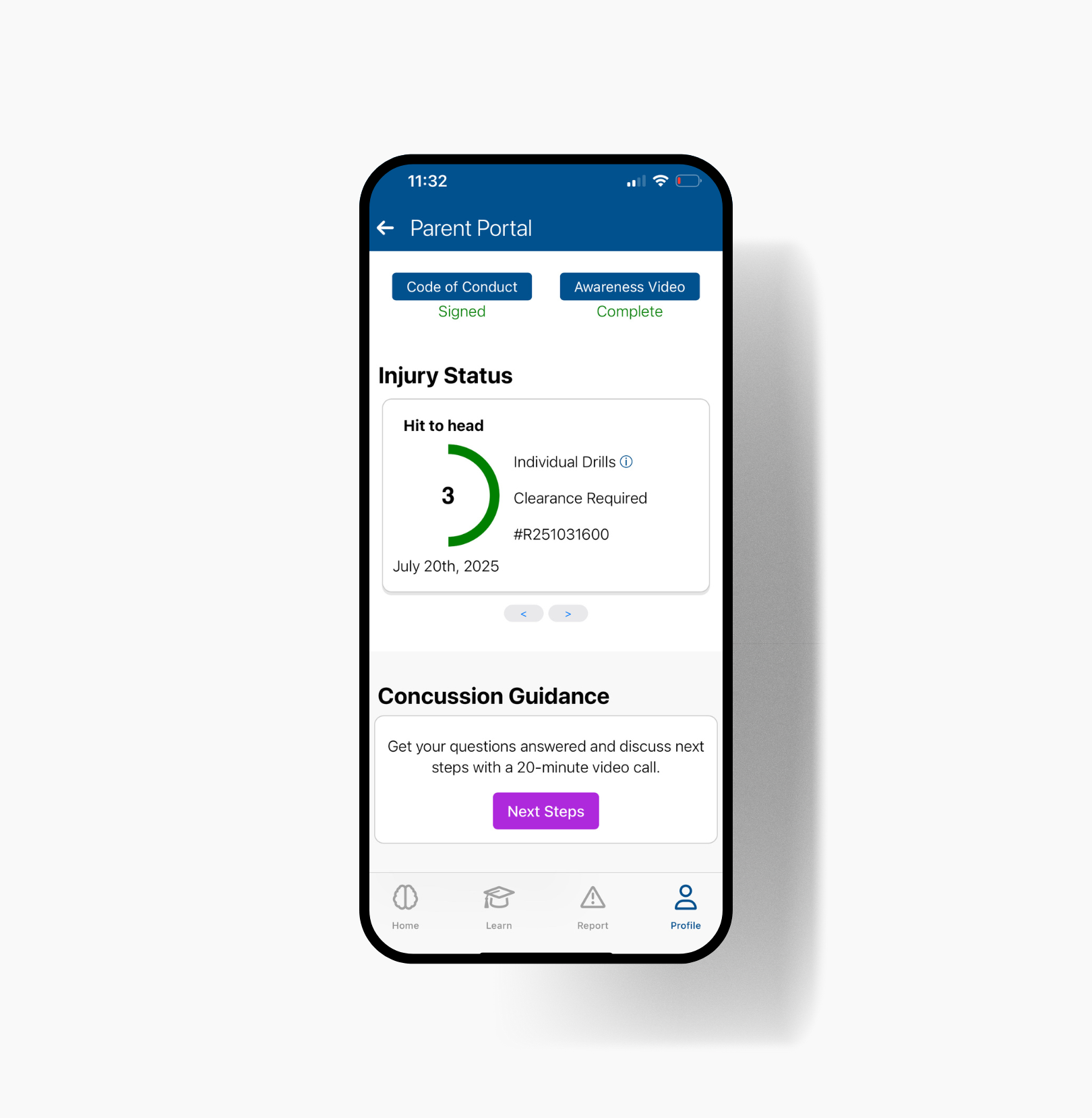
Immediate Response and Documentation:
When a concussion is suspected, CONCUSSIONALERT facilitates immediate, appropriate response:
- Real-time injury reporting by coaches or staff on-site
- Automatic notification to emergency contacts with clear next steps
- Secure documentation creating an electronic paper trail for legal protection
- Red flag symptom identification ensuring serious injuries receive emergency care
- Healthcare professional connection providing expert concussion assessment
Expert Healthcare Support:
Every athlete who reports concussion symptoms receives access to a free 20-minute virtual consultation with a Registered Kinesiologist who provides:
- Professional concussion assessment and education
- Guidance on concussion recovery and symptom management
- Referrals to local healthcare professionals for ongoing concussion treatment
- Peace of mind for parents during a stressful time
Safe Return-to-Play Management:
CONCUSSIONALERT manages the entire concussion recovery process, ensuring athletes don’t return to sport until fully healed:
- Step-by-step return-to-play after concussion protocol following evidence-based guidelines
- Symptom tracking throughout concussion recovery
- Medical clearance requirements before return to activity
- Follow-up report completion by coaches before athletes resume participation
- Final verification by Nurse Practitioners or physicians
Athletes cannot return to play after concussion until all protocol steps are complete and medical clearance is uploaded—removing guesswork and protecting both athletes and organizations from premature return-to-play decisions.
Protection for Organizations:
CONCUSSIONALERT protects sport organizations through:
- Rowan’s Law compliance with automated concussion education tracking
- Liability protection through comprehensive concussion management documentation
- Transparent communication with all stakeholders
- 10-year secure record retention meeting legal requirements
- Compliance insights showing organization-wide youth concussion safety metrics
Accessible for All Organizations:
Whether you manage a small recreational league or a large provincial sport organization, CONCUSSIONALERT provides affordable, scalable concussion management:
- Flat-rate pricing: $45/year or $5.99/month per athlete
- Unlimited coach accounts at no additional cost
- Quick setup: As little as 2 hours with required documentation
- 30-day onboarding: Most organizations fully operational within one month
- Multi-organization support: Athletes can link up to 2 organizations
Taking Action: Protecting Athletes from Concussion Risks
Understanding what is a concussion, recognizing concussion symptoms, and ensuring proper concussion recovery protocols is the foundation of athlete safety. When sport organizations combine concussion education with systematic concussion management tools, they create environments where athletes can pursue their passion while minimizing concussion risks.
Canadian sport organizations must comply with provincial concussion legislation, including mandatory concussion education, removal from play protocols, and medical clearance requirements for return to play after concussion.
CONCUSSIONALERT transforms concussion management from a compliance burden into a comprehensive safety system that protects athletes, educates stakeholders, and provides peace of mind for parents. By connecting coaches, parents, athletes, and healthcare professionals in one secure platform, CONCUSSIONALERT ensures every concussion receives the attention and concussion treatment it deserves.
Ready to enhance concussion safety and improve concussion recovery outcomes in your organization? Visit concussionalert.ca or contact support@concussionalert.ca to learn how CONCUSSIONALERT can help you prevent, recognize, and manage concussions effectively.
Knowledge protects. Preparation saves. CONCUSSIONALERT keeps athletes safe.
Related Resources